Healing Avoidant Attachment: An ACT-Led Guide to Secure Connection
Photo by Abigail via Unsplash
What is the most effective way to heal avoidant attachment?
Avoidant attachment heals through learning how to stay emotionally present without overwhelming your nervous system. Rather than forcing closeness or avoiding it altogether, change happens by understanding protective patterns, reducing fear-driven withdrawal, and practicing small, values-based steps toward connection at a pace that feels safe.
Key takeaways
Avoidant attachment is a protective response, not a flaw
Healing focuses on safety, flexibility, and choice
Skills-based approaches support gradual, sustainable change
Understanding avoidant attachment is an important first step, but changing these patterns often requires practicing closeness in real time, not just thinking about it. In attachment-focused therapy, I help adults work with shutdown, distance, and over-independence so connection feels safer and more flexible.
Explore attachment therapy for avoidant patterns.
What causes avoidant attachment in adults?
Avoidant attachment often develops when emotional closeness early in life felt overwhelming, unreliable, or discouraged (Bowlby, 1988; Mikulincer & Shaver, 2016). Over time, emotional self-reliance becomes a protective strategy that reduces distress by limiting vulnerability and dependence on others.
Knowing where these patterns come from can bring relief, but insight alone rarely shifts what happens in close relationships. In my work, therapy focuses on staying present during moments when your instinct is to pull away, while building skills for emotional safety and choice.
Learn how I treat avoidant and anxious attachment in therapy.
What are the signs of dismissive avoidant attachment?
Dismissive avoidant attachment often shows up as emotional distancing, discomfort with dependence, minimizing needs, and prioritizing independence over closeness, particularly during stress or conflict.
People with this pattern may value self-sufficiency and feel uneasy when others rely on them emotionally, even when relationships are otherwise meaningful.
How is fearful avoidant attachment different?
Fearful avoidant attachment involves a push-pull dynamic. Closeness is deeply desired, but it also triggers fear, leading to cycles of seeking connection and then withdrawing when vulnerability feels unsafe.
This pattern is often associated with heightened emotional sensitivity and confusion about whether closeness will bring comfort or harm.
Why does closeness feel threatening with avoidant attachment?
For avoidantly attached individuals, intimacy can activate nervous system threat responses linked to loss of autonomy or emotional overwhelm, even in safe relationships (Mikulincer & Shaver, 2016).
The body may react before the mind has time to assess the present situation, leading to shutdown, distancing, or emotional numbing as automatic forms of self-protection.
Can avoidant attachment be healed over time?
Avoidant attachment patterns can change through increased awareness, supportive relationships, and intentional practice within corrective relational experiences such as psychotherapy (Bowlby, 1988; Mikulincer & Shaver, 2016). Healing focuses on expanding tolerance for closeness rather than eliminating protective instincts altogether.
Progress is often gradual and shows up as greater emotional flexibility, clearer communication, and reduced reactivity during moments of intimacy or conflict. When avoidant patterns are rooted in developmental wounds, Sacramento complex trauma therapy can provide the collaborative structure needed for repair.
How do ACT skills support change in avoidant attachment?
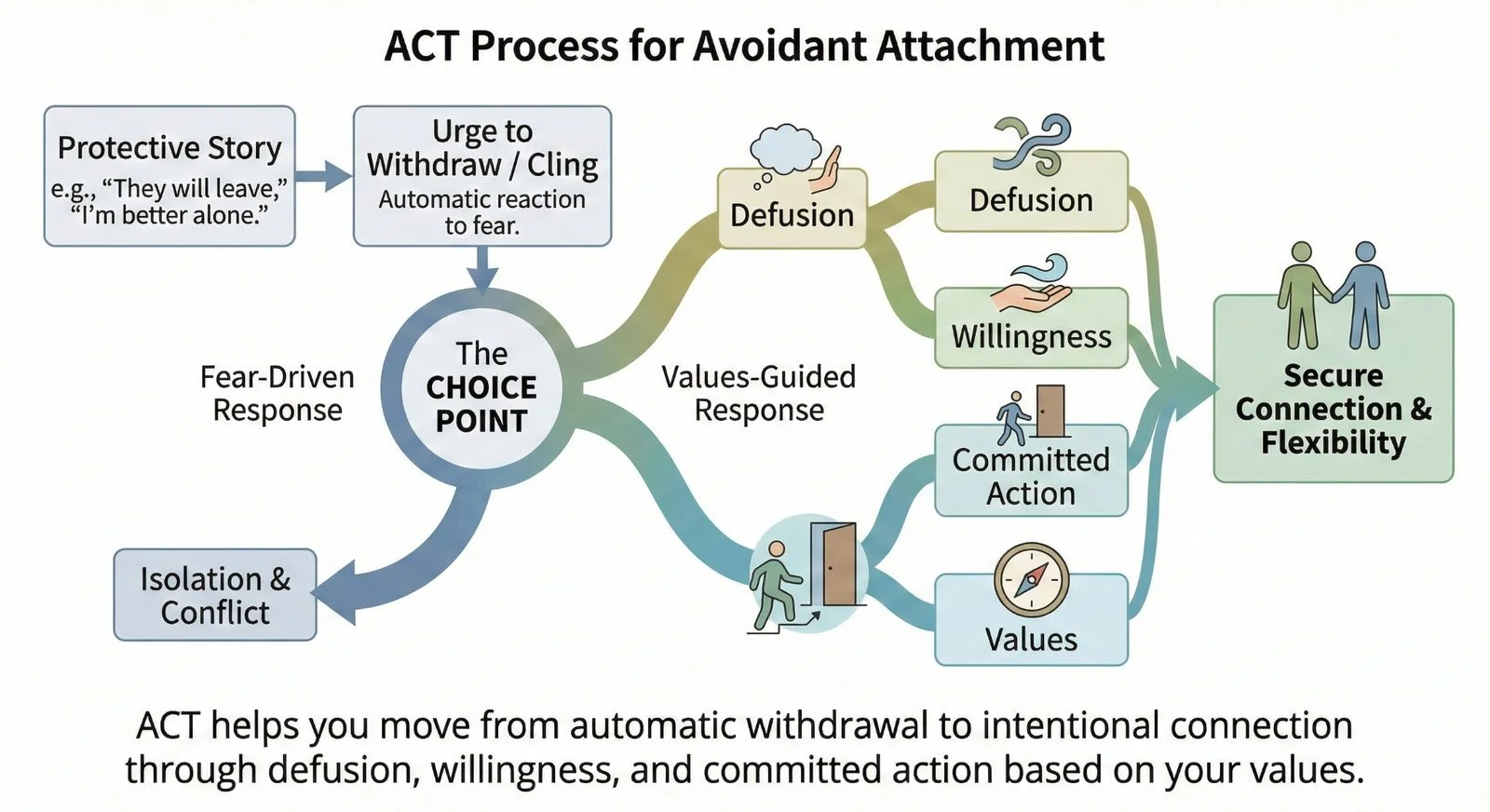
Acceptance and Commitment Therapy (ACT) supports change by helping individuals notice avoidance-driven thoughts, clarify values around connection, and take small, intentional steps toward intimacy without forcing emotional exposure (Hayes, Strosahl, & Wilson, 2012).
I use the ACT framework to help people move from automatic withdrawal to intentional connection. If you are ready to stop letting the urge to bolt run your relationships, you can learn more about my ACT-led approach for California and Virginia residents.
What does healing avoidant attachment look like in real relationships?
Healing avoidant attachment often looks like staying emotionally present a little longer, expressing needs more clearly, and tolerating discomfort without immediately pulling away.
Over time, relationships may feel less constricting and more collaborative, with space for both closeness and autonomy.
If you are recognizing this pattern in your relationships and want support changing it, therapy can provide a structured, compassionate space to practice closeness at your own pace. I offer attachment-focused therapy for adults who want connection without losing themselves.
Work with me for attachment-focused therapy.
If you want help, start here
• Who it’s for: Adults who recognize avoidant or anxious attachment patterns and want healthier closeness
• What we do: Attachment-focused, ACT-led therapy that prioritizes safety, pacing, and real-world relationships
• What to do next: Learn what therapy looks like and see if we’re a fit
For individuals in Northern Virginia, I offer Northern Virginia PTSD therapy with an attachment-informed lens.
Frequently Asked Questions About Avoidant Attachment
-
Some people experience shifts through supportive relationships and self-reflection, but therapy can provide structure, safety, and skills to support consistent change.
-
No. Avoidant attachment is a learned relational pattern that develops in response to early experiences and can change over time.
-
No. Healing focuses on flexibility and choice, allowing for both independence and closeness rather than replacing one with the other.
Ready to move toward secure attachment?
If you live in California or Virginia and are tired of the cycle of distancing and loneliness, let us see if attachment-focused therapy is a fit.
Further Reading & References
Further Reading (Helpful Resources)
These articles expand on key themes discussed above and may be helpful if you want to go deeper.
Acceptance and Commitment Therapy (ACT): What It Is and How It Works
ACT Therapy for Anxiety: How to Stop Struggling With Fear and Avoidance
CBT and Anxious Attachment: Understanding the Pattern and Treatment Options
PTSD and Relationships: How Trauma Impacts Closeness and Trust
These resources complement the discussion of avoidance, emotional safety, and values-guided connection without repeating the same material.
References (Research & Evidence)
The following sources support the concepts and claims referenced throughout this article.
Bowlby, J. (1988). A secure base: Parent–child attachment and healthy human development. Basic Books.
Mikulincer, M., & Shaver, P. R. (2016). Attachment in adulthood: Structure, dynamics, and change (2nd ed.). Guilford Press.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). Guilford Press.