ACT for Trauma: PTSD and Complex PTSD Without Reliving It
Quick Answer
Yes. Acceptance and Commitment Therapy (ACT) can help with PTSD and Complex PTSD by changing how you relate to trauma thoughts, memories, and body sensations. Instead of forcing you to relive the past in detail, ACT builds psychological flexibility so you can notice what shows up inside you and still choose how you want to live.
Here is the heart of it:
You do not have to tell your full story for ACT to be effective. We can work with what is happening in the present moment: triggers, body alarms, avoidance patterns, and the meaning your mind attaches to them.
ACT helps you step out of the avoidance loop that keeps PTSD symptoms going, with paced steps.
For Complex PTSD, ACT also targets toxic shame and identity pain, not just fear.
What ACT is: a skills-based approach that focuses on processes (attention, avoidance, values, self-compassion), not perfecting the content of your thoughts (Hayes et al., 2012; Arch & Craske, 2008).
What ACT is not: a promise to erase memories, a requirement to recount trauma in detail, or a one-size-fits-all replacement for trauma-focused treatments.
Related reading on my site:
Prefer video? Watch the short companion video below (includes a 60-second grounding practice).
Who this post is for
This post is for adults who:
Have PTSD symptoms (intrusions, avoidance, hypervigilance, sleep disruption) and want a meaningful and lasting, paced approach
Notice that avoidance has become the main coping strategy (numbing, overworking, staying busy, withdrawing)
Suspect Complex PTSD patterns like shame, emotional shutdown, or relationship disconnection
Need privacy or discretion (including high-responsibility professionals)
I provide online therapy across California and Virginia, with limited in-person sessions in Folsom, CA by appointment.
What this post does
Explains how ACT works for trauma in plain language
Helps you understand the difference between PTSD and Complex PTSD, especially the identity and shame layer
Gives a clear picture of what ACT sessions look like when trauma is in the room
Offers a paced next step if you want support
What this post is not
Not medical advice
Not a self-diagnosis tool
Not a crisis resource (if you are in immediate danger, call 911 or 988 in the U.S.)
Photo by Meriç Tuna via Pexels
Will I have to relive my trauma to heal?
Not necessarily.
Some trauma therapies are designed around directly processing the memory. ACT can be different. ACT is often a fit when the problem is not just the memory itself, but the pattern that grew around it: avoidance, numbing, hypercontrol, and living smaller to stay safe.
In ACT, we can work with:
What your mind says when you get triggered
What your body does (freeze, panic, shutdown, rage)
What you do next (avoid, isolate, drink, overwork, scroll, people-please)
What matters to you underneath all of that
Instead of asking, “How do we get rid of these thoughts or sensations?”, ACT asks a different question: “What happens when you try to control them, and what does it cost you?” That shift is often where healing starts (Hayes et al., 2012).
How ACT breaks the cycle of avoidance (the mechanism)
PTSD is not just fear. It is also a nervous system that learned danger fast, and a life that slowly reorganized around not feeling it.
ACT targets the avoidance loop directly. Here is the simplest version:
Trigger (a sound, a look, a memory, a body sensation)
Alarm (intrusion, panic, numbness, shame, rage)
Avoidance or control (escape, shutdown, substances, overthinking, reassurance seeking)
Short-term relief
Long-term cost (more fear, more stuckness, less life)
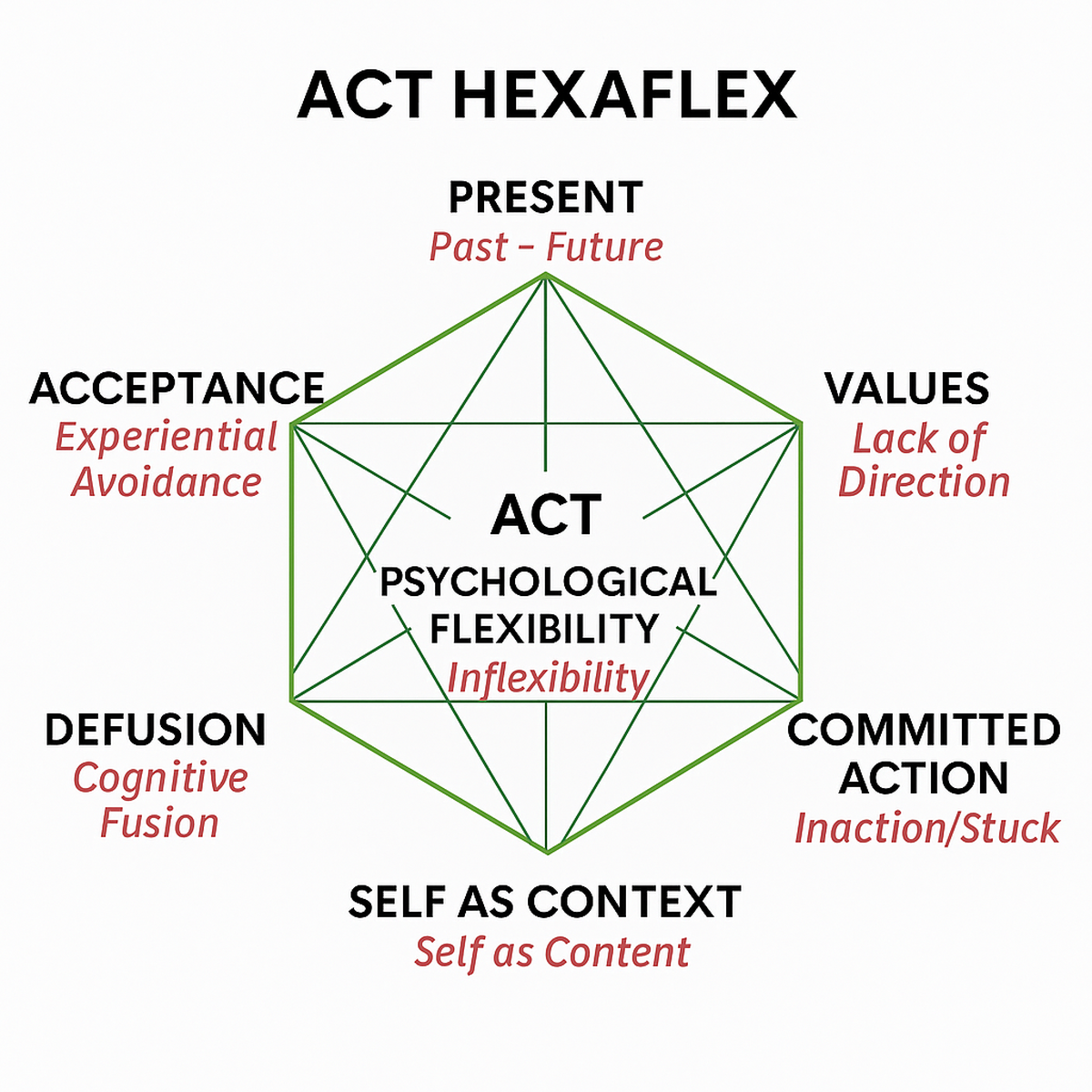
ACT helps by strengthening six core processes of psychological flexibility (Hayes et al., 2012):
Copyright Steven C. Hayes. Used by permission.
Present-moment awareness: orienting to “right now” when the body is pulled into “then”
Defusion: noticing thoughts as thoughts (“My mind is telling me…”) instead of facts
Acceptance/willingness: making room for sensations long enough to act with choice
Self-as-context: remembering you are more than your trauma story or symptoms
Values: clarifying what matters so fear, anxiety, or self-protection are not the only compass
Committed action: taking sustainable steps that rebuild your life
This is a process-based model. We are not trying to debate whether a trauma thought is “true.” We are changing the impact it has on your body and your behavior (Arch & Craske, 2008; Hayes et al., 2012).
What ACT looks like in real life
Instead of “Tell me everything that happened,” an ACT approach might sound like:
“When your body spikes, what do you do next?”
“What would your life look like if anxiety was no longer in charge?”
“Can we practice staying with a wave of sensation for 20 seconds and then choose your next move?”
This is not avoidance disguised as therapy. It is paced exposure to the present, anchored in values.
Evidence note: ACT has growing use as a trauma-informed, process-based therapy for people struggling with trauma-related symptoms such as avoidance, emotional distress, and difficulties staying engaged in daily life. It is often chosen when individuals want an approach that emphasizes psychological flexibility, pacing, and values-based change rather than intensive trauma retelling. Research in this area is still developing, and ACT is not a universal first-line fit for every person.
ACT for Complex PTSD: healing shame and identity (not just fear)
Complex PTSD (CPTSD) is included in the ICD-11. It involves PTSD symptoms plus disturbances in self-organization: emotion dysregulation, negative self-concept, and relationship difficulties (Cloitre et al., 2013; National Center for PTSD, 2025).
For many people, the most painful part is not only hypervigilance or flashbacks. It is:
“I am broken.”
“I ruin relationships.”
“I don’t deserve care.”
ACT can be powerful here because it works directly with identity fusion and toxic shame.
1) Unhooking from shame stories
Shame is sticky because it sounds like truth. ACT teaches you to notice shame as a mental event, not your identity. A small shift like “I’m having the thought that I’m unlovable” can create enough space to choose something more workable.
2) Self-as-context: you are more than what happened
Trauma can collapse identity into a single storyline. ACT strengthens the “observing self,” the part of you that can notice fear, shame, and numbness without being defined by them (Hayes et al., 2012).
3) Values-based reconnection
Complex PTSD often includes relationship pain: distancing, distrust, or people-pleasing to stay safe. Values work helps you define what healthy connection looks like for you (trust, honesty, boundaries, steadiness) and practice it in real, doable steps.
Pacing your nervous system: staying inside your window of tolerance
A trauma-informed ACT approach prioritizes pacing.
When your nervous system is outside its workable zone, your options shrink. This is why trauma work can feel like either:
Too much (panic, overwhelm), or
Not enough (numbness, shutdown)
In ACT, we practice skills that help you stay with experience in a tolerable way:
Grounding and orienting (what I see, what I hear, what is safe right now)
Noticing urges to escape and choosing a smaller, safer step
Building capacity progressively
The goal is not forcing or resisting. The goal is flexibility.
Values-based recovery: building a life bigger than trauma
Trauma can turn life into management: managing symptoms, managing triggers, managing other people’s reactions.
ACT adds a missing ingredient: direction.
Values are not goals you can check off. Values are qualities of living you can practice repeatedly, even while healing. Examples:
Being present with my kids
Integrity in my work
Courage in relationships
Caring for my health
When values are clear, fear is no longer the only decision-maker. This is the heart of committed action (Hayes et al., 2012).
Is ACT right for me if I have PTSD or Complex PTSD?
ACT may be a strong fit if:
You are exhausted by fighting your mind or body
Avoidance has become automatic
You want skills you can use in the moment, not just insight
Shame and self-judgment feel central to your trauma experience
You might consider a different approach (or a combined plan) if:
You specifically want structured trauma memory processing right now
You are seeking a highly manualized trauma protocol as your primary path
Many clients benefit from integrating approaches over time. What matters is choosing a plan that matches your needs, readiness, and nervous system capacity.
If you are looking for online trauma therapy in California or Virginia, you can also explore my service pages:
Next step
If this approach feels like it fits, a good first step is a short consultation where we clarify:
What you are dealing with right now (symptoms, triggers, avoidance patterns)
What you want your life to stand for, even while healing
What kind of pacing and structure would feel safe and workable
You can reach me here: Contact
Further Reading & References
Further Reading (Helpful Resources)
U.S. Department of Veterans Affairs, National Center for PTSD. (2025). ACT Coach mobile app.
U.S. Department of Veterans Affairs, National Center for PTSD. (2025). Complex PTSD: Assessment and treatment.
U.S. Department of Veterans Affairs, National Center for PTSD. (2025). Complex PTSD: History and definitions.
Walser, R. D., & Westrup, D. (2007). Acceptance and commitment therapy for the treatment of post-traumatic stress disorder and trauma-related problems: A practitioner’s guide to using mindfulness and acceptance strategies. New Harbinger Publications.
Acceptance and Commitment Therapy (ACT): How It Can Help You Heal
References (Research & Evidence)
Arch, J. J., & Craske, M. G. (2008). Acceptance and Commitment Therapy and Cognitive Behavioral Therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice, 15(4), 263–279.
Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4 (Suppl 1), 20706.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). Guilford Press.
National Center for PTSD. (2025). Complex PTSD: History and definitions. U.S. Department of Veterans Affairs.
Frequently Asked Questions
-
ACT is an evidence-based therapy with growing support for trauma-related difficulties such as depression, anxiety, avoidance, and emotional regulation challenges that often accompany PTSD. Rather than focusing on retelling traumatic events, ACT works on helping people relate differently to distressing thoughts, emotions, and body sensations so they can move toward a meaningful life. ACT has been widely used with Veteran populations, first responders, and other high-stress professionals, in both individual and group formats. The best approach depends on your needs, goals, and readiness.
-
No. In ACT, we can work primarily with the present-moment impact of trauma: triggers, avoidance, nervous system responses, and the meaning your mind attaches to them.
-
ACT is focused on changing your relationship with internal experiences (thoughts, sensations, memories) so you have more choice and flexibility. It can include paced, values-guided exposure to life, but it is not always centered on revisiting the trauma memory.
-
Yes, ACT explicitly targets identity fusion, self-judgment, and the stories the mind builds after chronic trauma, while also supporting emotion regulation and reconnection.
-
Yes. The VA’s National Center for PTSD offers ACT Coach, a free app designed to support ACT skills practice alongside treatment.
-
Yes. I provide secure telehealth for adults across California and Virginia, with limited in-person sessions in Folsom, CA by appointment.